Healthcare in Our Community
2026 Survey Highlights &
Town Hall Summary
The 2026 Healthcare in Our Community Survey was conducted as a follow-up to the 2023 survey, which captured a period of significant stress in local healthcare.
The intent of the 2026 survey was to:
Understand what has changed since 2023
Identify where pressures remain or have increased
Ground local planning and advocacy in current community experience
The results were shared publicly at a community town hall to ensure transparency and dialogue.
Below are the survey results and key messages shared at the Town Hall on February 2, 2026.
Survey at a Glance
128 respondents (2026)
📈 More residents accessing care locally
🤝 Increased trust in care
⏱️ Growing demand
🚑 ER access remains top concern
2023 to 2026 What’s Changed?
2023:
86% of people were seeking primary care out of community,
concerns over competency,
system instability,
loss of trust,
ER closure frustrations
2026:
63% of people seeking primary care in community,
improved quality of care & provider trust,
higher demand for services,
concerns with timely appointments,
ongoing frustrations with ER closure
In 2023:
86% of respondents were seeking care outside of Consort due to lack of trust and concerns over quality of care
Of those surveyed regarding care they had received at the clinic:
48% rated their care Poor or Very Poor
35% rated the care as “Fair”
17% rated the care as Good or Very Good
The results of the 2026 survey are clear - things have improved since 2023 in relation to primary care services in our community.
The responses demonstrate a vast improvement in:
•Quality of primary care
•Trust in providers
•People seeking care in community
That doesn’t mean everything is perfect — and we’ll talk about the challenges, gaps, and frustrations that were noted in the survey — but it is important to acknowledge that progress has been made.
The survey responses were very clear on this point.
What Has Improved Since 2023
In 2026, results showed:
Increased Trust in Local Care
Respondents consistently described local primary care as:
High quality
Respectful
Patient-centred
Consistent
Trust in Nurse Practitioner-led care was one of the strongest positive findings in the survey.
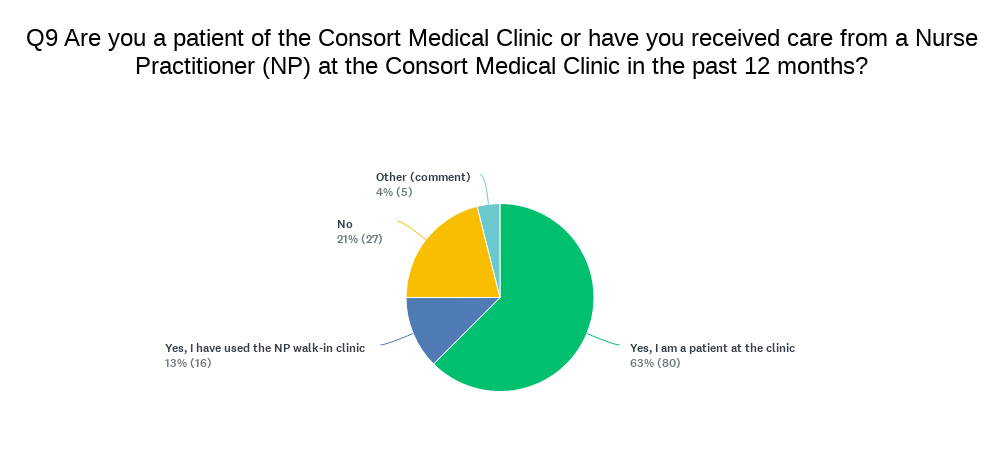
63% of respondents are patients of the Clinic,
13% of non-clinic patients are using the NP walk-in clinic
and many of the "no" or "other" responses are due to being waitlisted or out of the current service area.
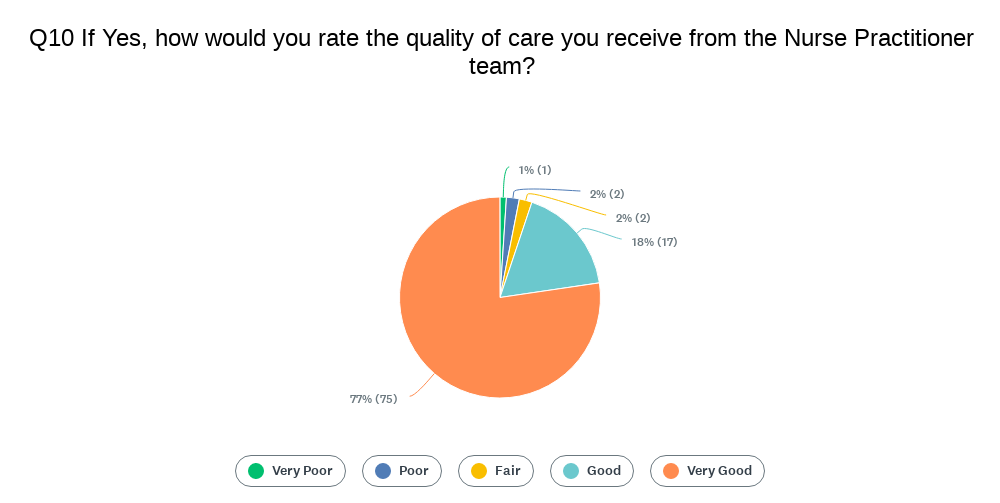
5% rated care as Fair or below
95% rated care as Good or above (77% was the highest option of “very good”)
NP/Weekend Walk-In Clinic
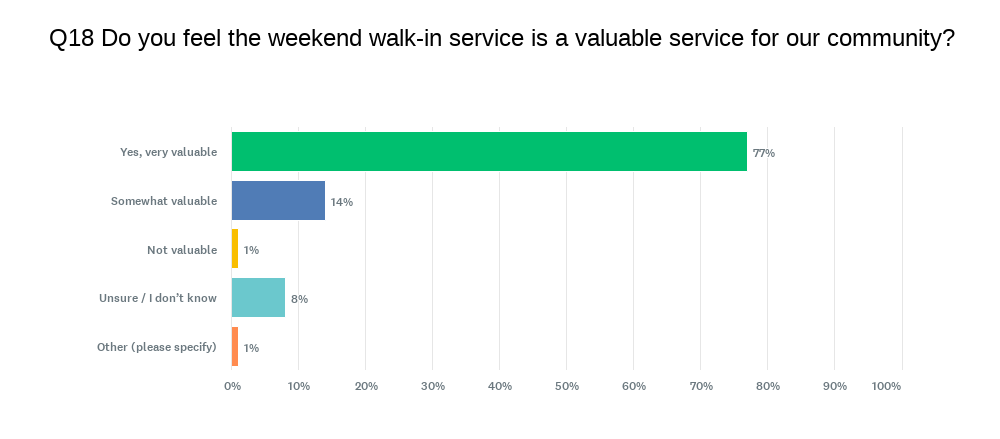
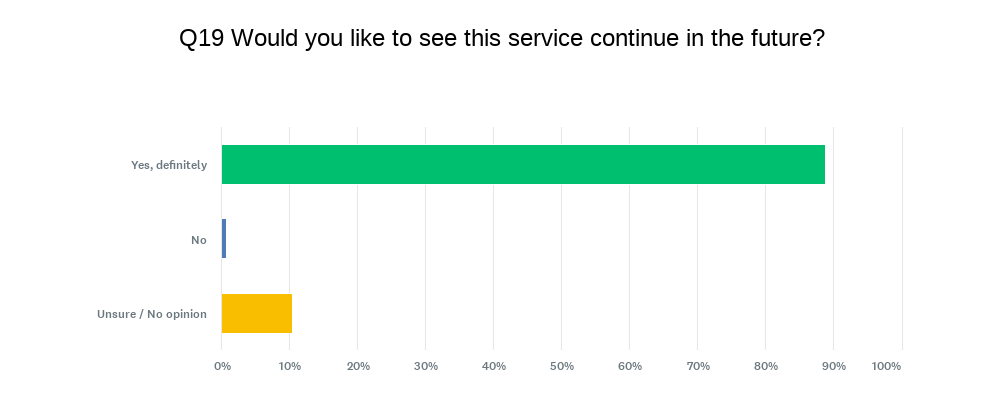
The majority of respondents indicated that:
The weekend walk-in service is valuable
There is strong support for continuing the service in the future
The survey shows strong trust in NP care and our team-based model. People told us they feel listened to, respected, and confident in the care they’re receiving.
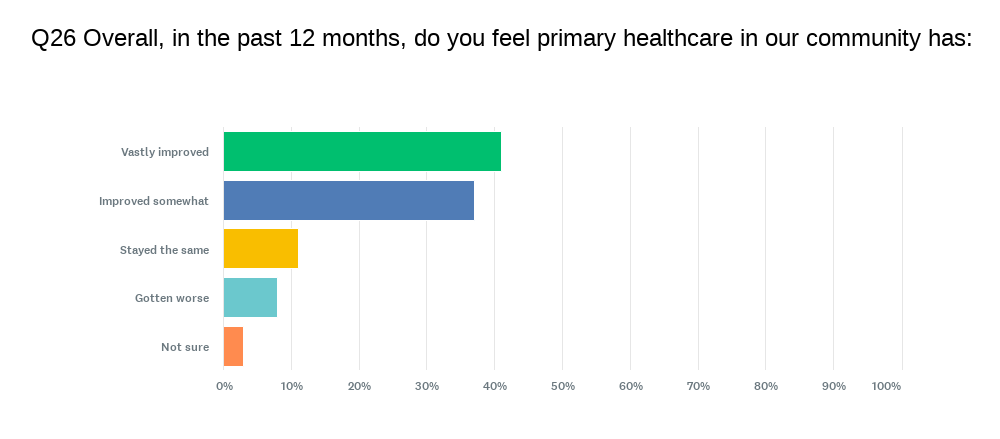
Overall, 78% think primary care has improved over the past 12 months
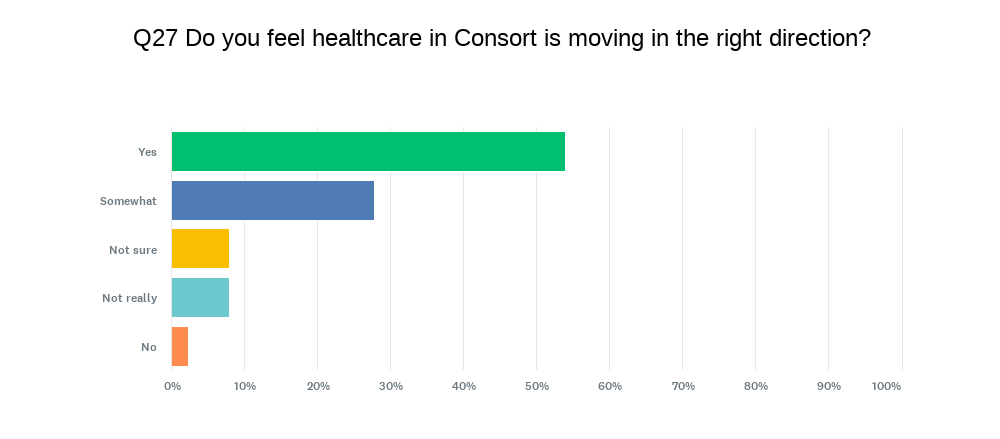
And while 54% of people think healthcare is moving in the right direction, access to ER or urgent care still remains the largest concern.
Now, it is important to remember, improvement doesn’t mean perfection.
In fact, one of the reasons we’re seeing new frustrations — like less appointment availability, longer wait times when booking appts, or being placed on an intake waitlist — is because more people are using the clinic now than they were in 2023, combined with the fact that NPs practice differently and appt times are longer so less people are able to be seen in a day.
Better care leads to higher demand.
That’s a good problem to have — but it’s still a problem we need to address.
And that’s where the conversation shifts from what’s improved to what’s under pressure.”
WHICH DECISIONS ARE UNDER LOCAL CONTROL?
The Medical Board Does Control
Primary Care Clinic/Medical Clinic
Clinic operations & staffing
Local planning & partnerships
The Medical Board Does Not Control
Emergency Department services
Hospital operations/closure decisions
Ambulance and EMS coverage
Why Understanding This Matters
From the outside, it can all feel like one system.
But in reality, the decision-making regarding our local healthcare services is a complex, and often convoluted system to navigate.
A lot of frustration lands at the Clinic or the Medical Board because they’re the most visible.
But understanding where decisions actually get made helps us direct that frustration — and advocacy — where it has the best chance of making an impact.
Advocacy around emergency services hasn’t stopped — it’s ongoing. The survey results are a big part of that. They give us concrete evidence of how the lack of emergency access affects this community.
It’s important to say this clearly: any actions or initiatives to improve primary care do not mean we’ve given up on pushing for reinstatement of our emergency services.
Strengthening our primary care services and increasing the number of healthcare services and providers in the community gives us more leverage in our advocacy efforts.

Emergency Services Remain the Largest Concern
Despite improvements in primary care, lack of Emergency Department access remains the community’s top concern.
74% of written responses referenced concerns about ER access
83% identified the return of ER services as the single most impactful change for local healthcare
This concern has remained consistent across both surveys.
Just like in 2023, the absence of local emergency services remains the single biggest concern people raised.
The need for access to ER hasn’t changed — strong primary care can’t replace emergency services.
Survey responses remained very similar to results from 2023
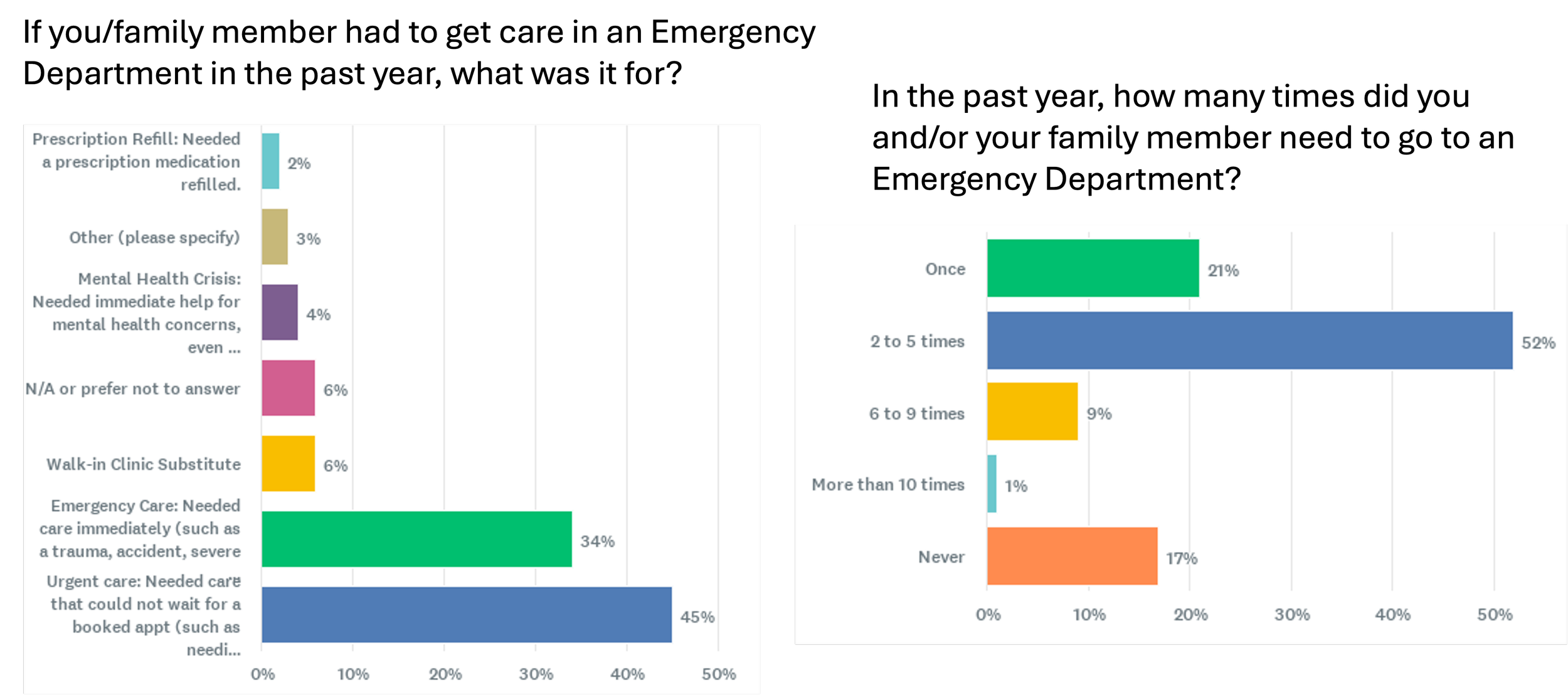
79% of those surveyed reported being seen in an ER for emergency or urgent care concerns
34% Emergency Care: Needed care immediately (such as a trauma, accident, severe injury, chest pain, stroke, seizure, very sick child, asthma attack, fractured bone, pre-term labour, fever in cancer patients)
45% Urgent care: Needed care that could not wait for a booked appt (such as needing stitches, abdominal pain, prolonged cough, sick child, feeling generally unwell)
52% of respondents accessed ER 2-5x
With 81% of respondents accessing ER services at least once
Most utilized ER depts by respondents are:
Provost: 35%
Coronation: 19%
Castor: 10%
Oyen: 8%
Wainwright: 8%
Hanna: 0%
“Other”: 10% and often included responses of a combination of Provost, Coronation, Castor or Wainwright
The survey also made clear that progress has brought new challenges.
Where Pressures Have Increased
Appointment Availability
As more residents seek care locally:
Demand has increased
Wait times for non-urgent appointments have lengthened
Frustration with waitlists has grown
We heard a lot of frustration about how long it can take to get an appointment.
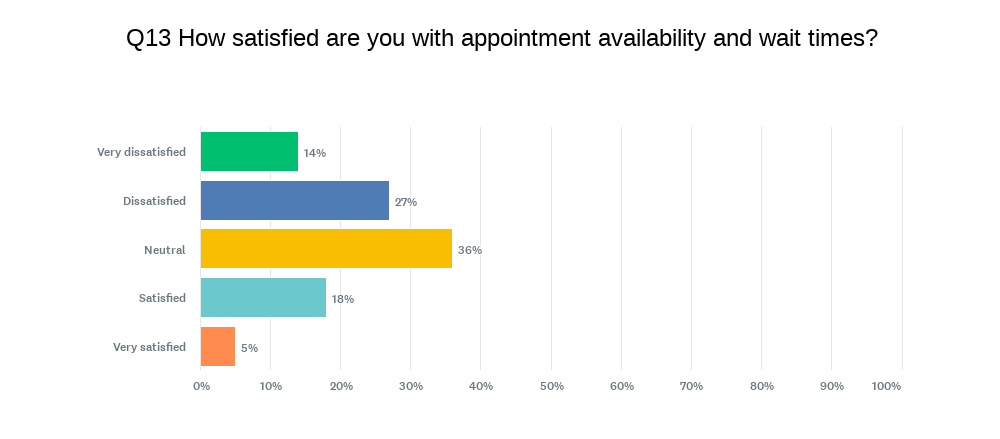
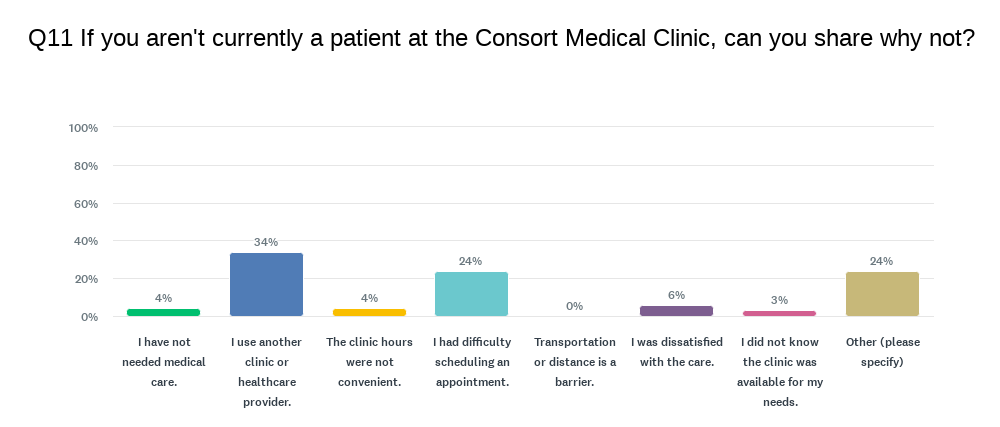
41% of respondents are dissatisfied or below with appointment availability and wait times btwn appts
43% report difficulty getting an appt in a timely matter as a barrier to care
And 29% site limited availability of healthcare providers are a barrier to accessing primary care.
Another thing people talked about was the challenge of more urgent primary care needs such as bladder infections, sore throats, kids with ear aches, etc.
When appointments are full and there’s no after-hours option locally, people are left with tough choices: wait, travel to a nearby ER, or hope it gets better. None of which are good options.
When you’re sick, in pain, or worried, waiting feels unacceptable.
Those frustrations are real — and they’re valid.
We want to acknowledge that we have heard your concerns and frustrations and are working to find solutions that work for our clinic and our community.
And we ask that we all try and remember that our providers and the staff at our clinic are humans doing the best that they can in a very tough situation.
NPs practice differently than physicians, and their model is not built around volume of patients seen in a day.
A lot of work happens outside of the exam room. Each patient visit usually has an average of an additional 20-40 minutes of charting, referrals, consultation work, or research involved.
With new patients, there is usually 40-90 minutes involved outside of “seeing the patient” to ensure medication records are up to date, patient history is properly charted, screening and prevention protocols are in place, plus putting together a care plan for the new concerns brought forward during the initial visit.
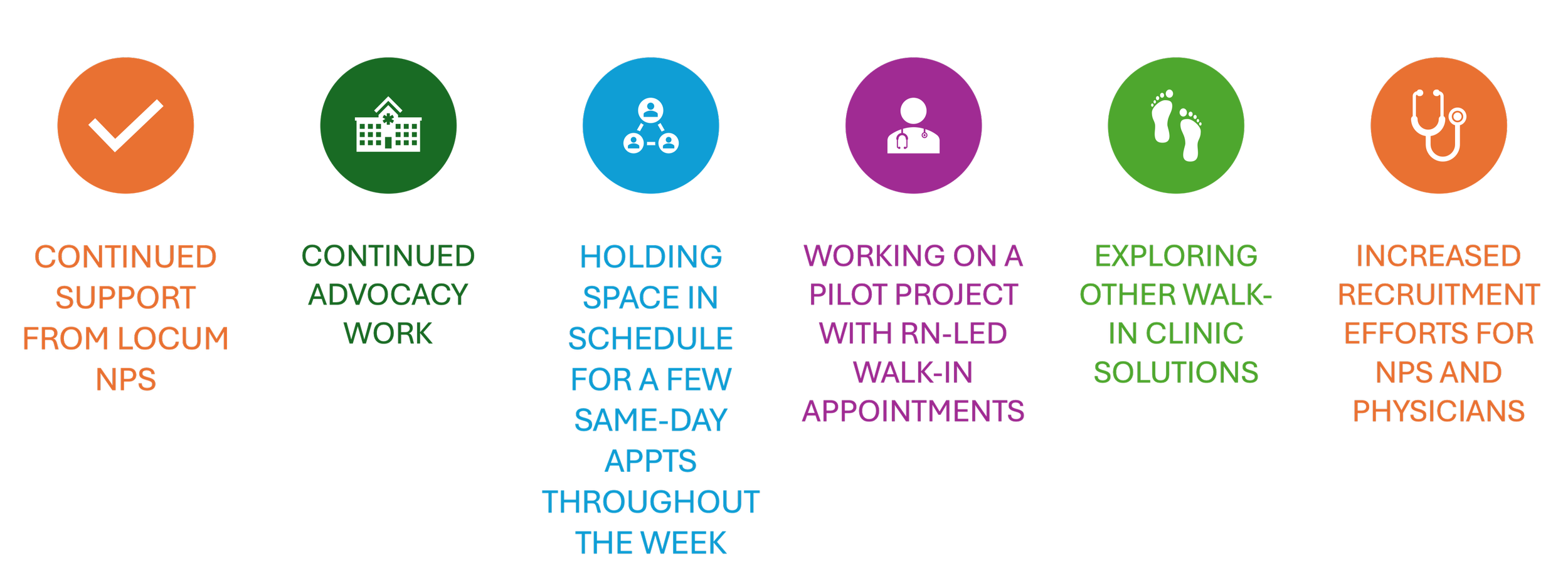
We understand that the part-time and locum NPs are only a piece of the puzzle, and that more full-time support is needed.
We also heard frustration about same-day appointments. The clinic is working hard to accommodate more urgent primary care needs where possible — but with limited providers, not every concern can be handled same-day, even when it feels urgent.
It is also important to remember that the clinic is not equipped to handle emergencies or conditions that require medical interventions like oxygen, IVs, etc.
We are also limited by the fact that most of the labs that would be required to assist with diagnostics for certain conditions aren’t available for in-house results, meaning, while labs are collected here, they are transported out every day for processing.
If the provider feels that labs are needed to help diagnose you in an urgent manner, they have to send you to ER for those fast results regardless.
At this current time, our NPs are not privileged to provide care or send orders with a patient to ER, so there is no way to “shorten” ER wait times by coming to clinic first.
Triage decisions about same-day appts are made based on clinical capacity, the level of support needed, and best practice guidelines. We understand that it is frustrating to not be seen same-day or to be told you must go to ER when you feel it could be handled locally.
Steps we are taking to address the problem
Key Message From the Town Hall
One message was emphasized throughout the presentation:
Improvement does not mean perfection.
The survey reflects real progress in local primary care, alongside real and ongoing challenges — particularly related to capacity pressures. We understand that people are frustrated, and those frustrations are valid.
We are working on solutions that we hope will not only address the needs of patients, but also of our healthcare providers. We are committed to keeping patients and the community at large updated through regular articles in the paper and updates on social media and through our patient messaging portal.
All provider solutions aside, we still face one critical barrier
Space/Physical Capacity
Simply put, we are over-capacity for space most days of the week – with no room to grow.
Our current clinic space limits:
- how many providers can work at the same time,
- how many appointments we can offer in a day, and
- what services we can realistically add.
Even if we had more providers available tomorrow, we don’t have the space and exam rooms to effectively support them.”
It’s also important to put this in context. Communities around us — Oyen, Hanna, and Provost — all now, or will very soon, be operating out of modern, stand-alone clinics. That gives them a real recruiting advantage. Providers are looking for environments that support team-based care, and are clean, safe, and efficient.
When you put all of this together, the picture looks like this:
Clinic is being utilized more.
Current providers are stretched.
Our model of care is working — but it’s over-capactity.
Appointment wait times are too long, the waitlist for care continues to grow, and people are frustrated.
That doesn’t mean our model is broken.
It means we’ve reached the limits of what our current setup can handle.
The solution isn’t to rush care or shorten appointments. The results show people are happy with the care they are receiving. This isn’t about changing what’s working.
At this point, the question isn’t whether quality care will be utilized if it’s available — it’s whether we create the capacity to meet the demand.
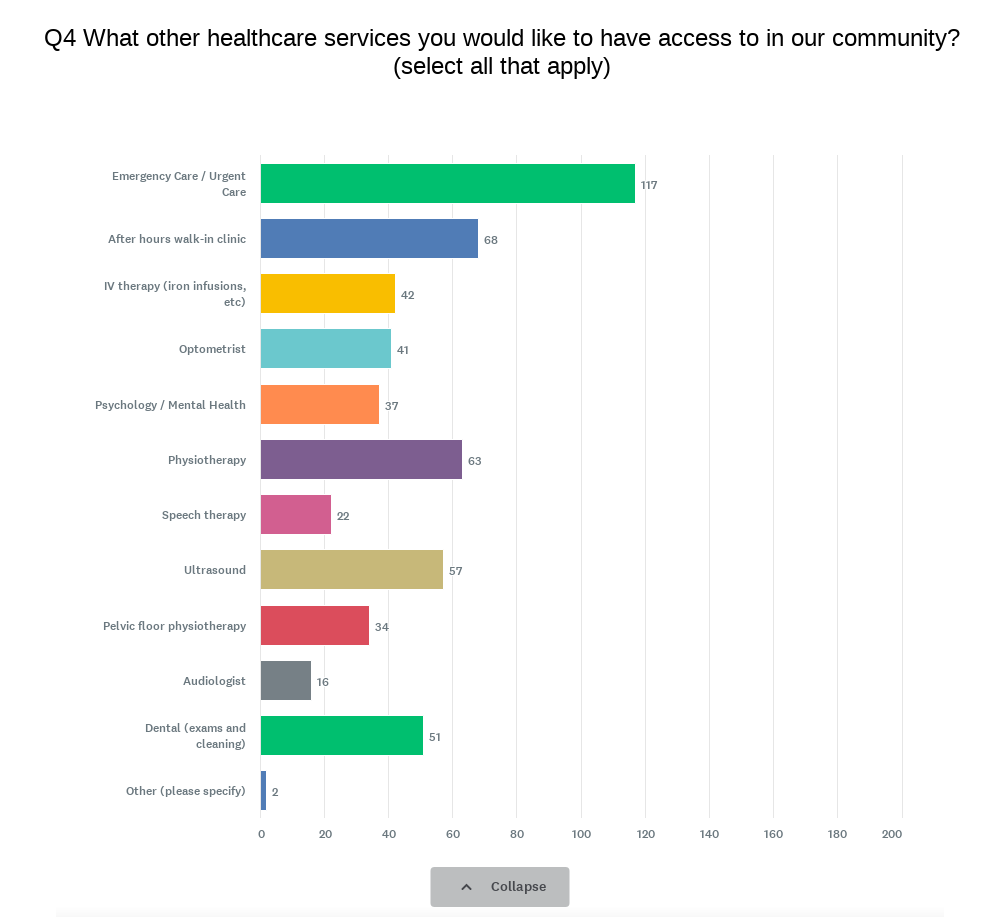
The community sees value in having access to a variety of services locally.
One of the responses, the IV therapy clinic is something we have received grant funding to start up, but in our current clinic space is an issue so we are trying to navigate how we best implement that with the space we have.
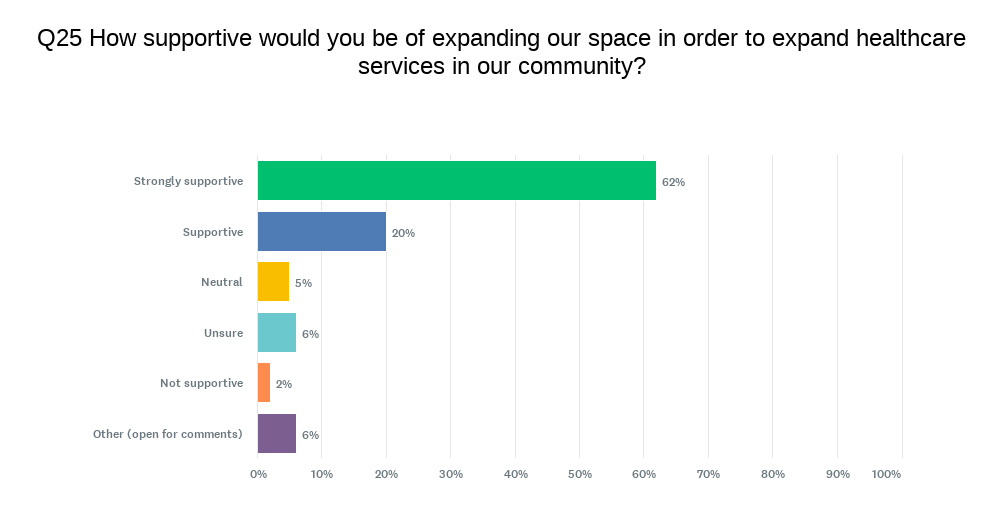
How supportive would you be of expanding our space in order to expand healthcare services in our community?
82% of respondents were supportive of clinic expansion to meet the needs of the increasing demand and to aid in our recruitment efforts.
6% of respondents left comments that they would support an expansion but wanted to make sure it was still in the hospital.
REALITIES OF OUR CURRENT SPACE
The Consort Medical Clinic rents space in the Consort Hospital. We do not own our space, nor do we have control over renovation, maintenance, or upkeep decisions.
Summer 2025 we had a leak in the roof where a large light sits above our staff kitchen sink. It’s still hanging by chains despite numerous requests to fix it over the past 8 months.
I would like to point your attention to the staff bathroom “door”, it’s a locker door style bathroom which leaves about a foot of space at the bottom of the door. The sink for handwashing from the bathroom is the kitchen sink. We can’t have the microwave, coffee maker and fridge all plugged in at the same time because there are not enough outlets.
There are 3 functioning exam rooms, which for the NP model is workable but tight. This does not work for physicians, as they usually run 2 rooms at a time.
We are simply outgrowing the space and there is no where to expand into.
The renovation approval process and the associated costs are key deterrents in expanding where we are.
It is very hard to recruit providers into a space that is over-capacity at best, and unsafe at worst.
When we bring this back to the survey, the message is clear.
People want better access.
They want shorter wait times.
They want more services available locally.
Space doesn’t solve everything — but without it, many of the improvements people are asking for simply aren’t possible.”
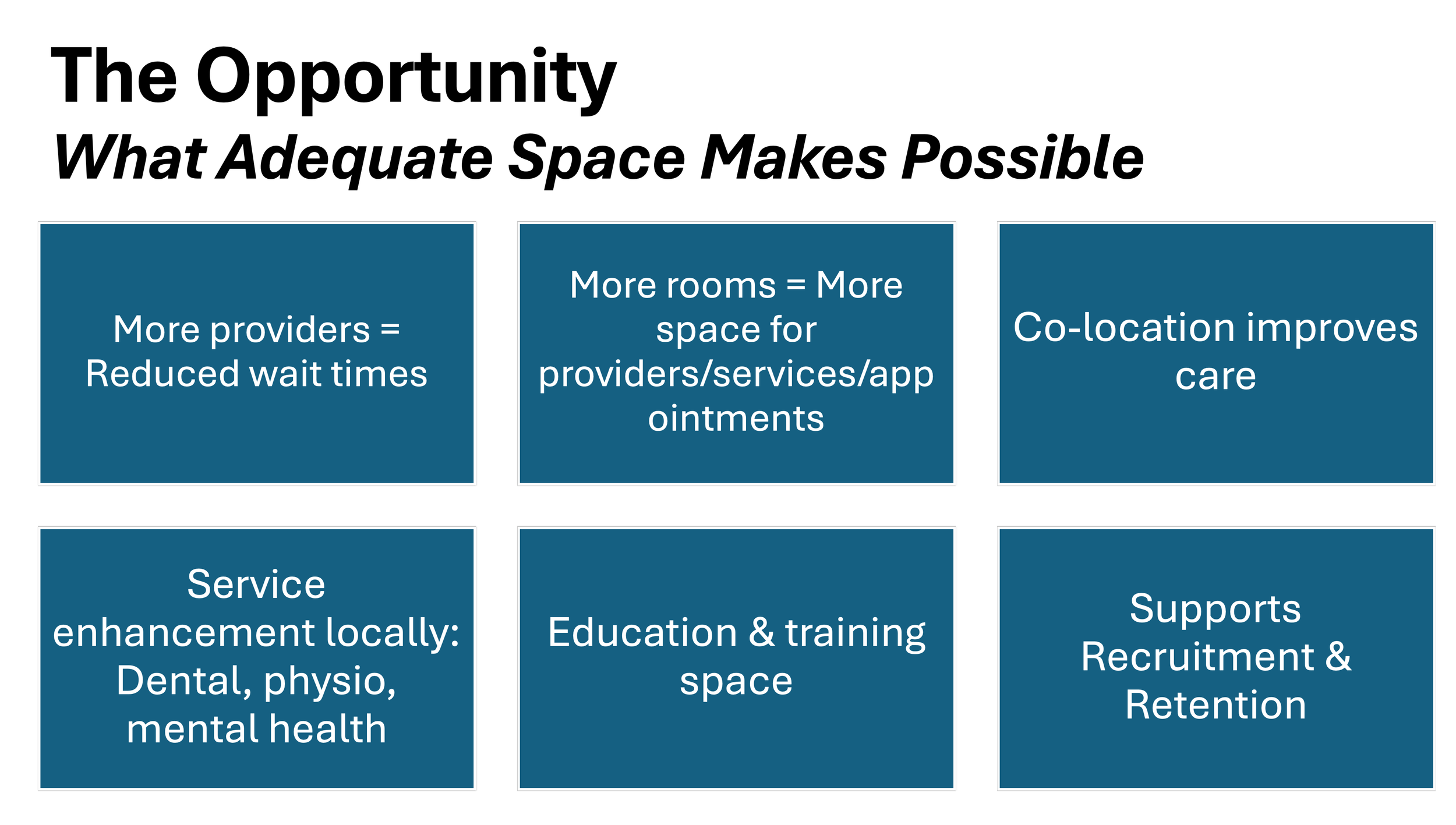
The Opportunity
Over the past several months, the Consort Medical Board & Clinic have been having conversations about our clinic space and the restrictions we are facing in terms of additional provider capacity and recruitment efforts.
Our space limits how many providers we can bring in, how many appointments we can offer, and what services we can realistically add — even though the demand is clearly there.
As a result of those conversations, the CCR building has been gifted to the community as a donation for healthcare use.
We want to acknowledge the generosity behind that offer. It reflects a genuine commitment to supporting local healthcare and one that allows us to seriously consider how we address the space constraints we’re facing, as well as the vision for primary care in Consort.
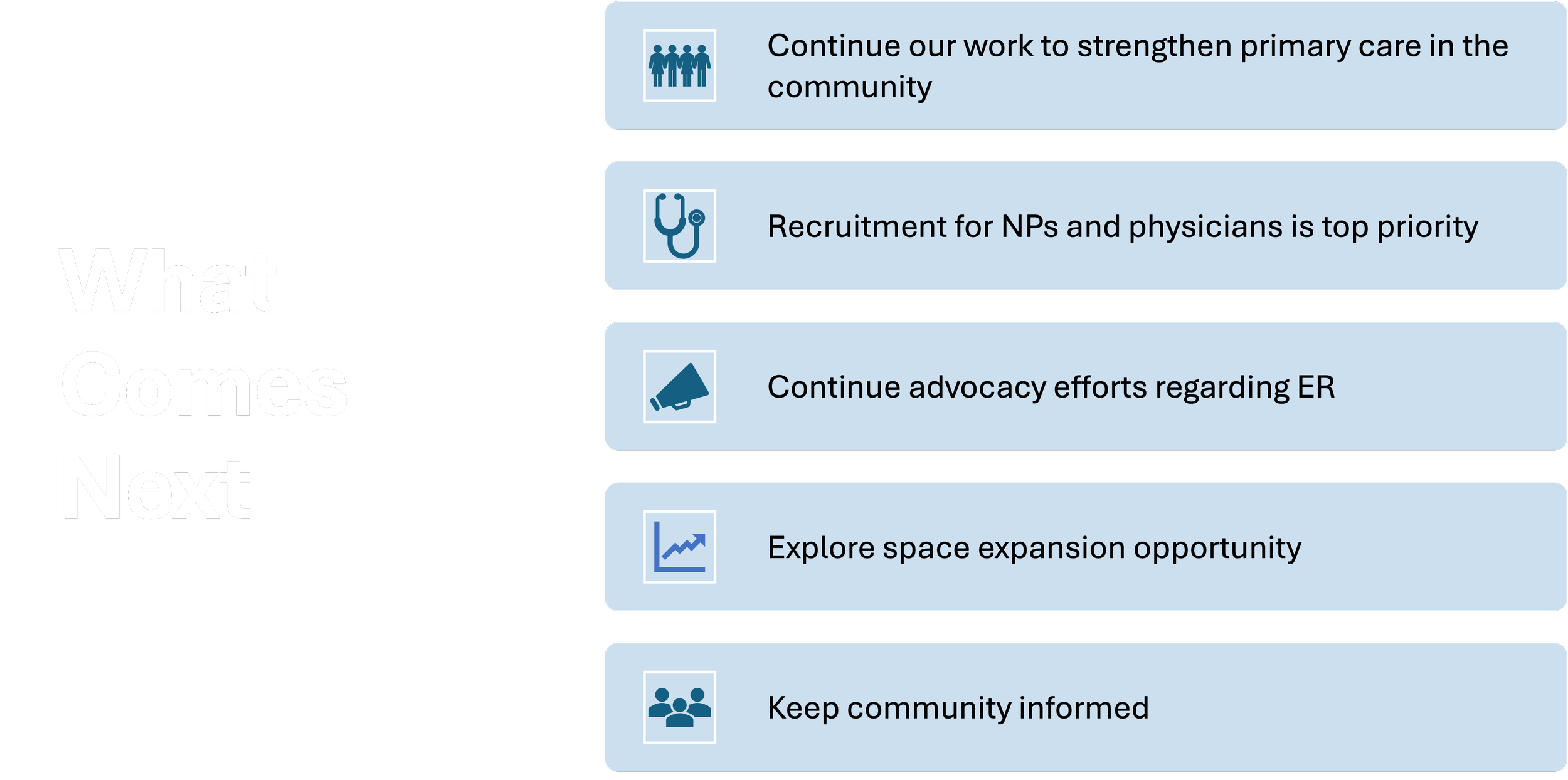
It’s also important to be clear about what this does not mean. This is not about abandoning our push for emergency services and enhanced lab and x-ray services.
The advocacy work continues regardless of where we are located — and emergency services remain a top priority for this community.
“The question isn’t whether healthcare needs to grow — it’s how we create the conditions for it to grow well.”
Rural healthcare works best when growth is intentional, not reactive.
The future vision isn’t about starting over.
It’s about building on what’s already working — strong Nurse Practitioner care, trusted providers, and a community that’s using local services again.
The foundation is there. What’s missing is room to grow.
A comprehensive primary care centre — a place where Nurse Practitioners, physicians, nurses, and allied health providers can work together — not in silos, but as a team.
The survey and ongoing conversations point to the same thing: people want fewer reasons to leave the community for care. Co-locating services like mental health and counselling, physiotherapy, and dental care helps reduce travel, reduces stress, and keeps care connected.
These services don’t replace hospitals or specialists — they support primary care and prevent issues from escalating.
This is about planning for the community we’re becoming — not the one we were 20 years ago.
Our future vision comes back to three things:
Access — people being able to get care when they need it.
Stability — providers and services that stay.
And sustainability — building a healthcare system that can support this community now and into the future.
Questions about the survey results or the Town hall meeting?
Email: admin @ consortmedical.ca